You just aren’t feeling well, so you head to the doctor, thinking an antibiotic might do the trick. But the doctor says an antibiotic won’t help. Why is that?
There are a lot of misconceptions out there about antibiotics. These powerful medications, also called antibacterials, have played a key role for decades in treating illnesses.
But they aren’t the be-all, end-all — they’re only appropriate for treating bacterial infections, not viruses.
Here’s what you should know about antibiotics and their role in keeping you healthy.
Antibiotics: Yes for bacteria, no for viruses
Many people head to the doctor when they’re experiencing symptoms related to the respiratory system. But in the vast majority of cases, those types of symptoms come from viruses, not bacteria.
That means that antibiotics, which treat bacteria, would be ineffective. Antibiotics won’t treat:
- The common cold
- The flu
- A runny nose
- Most sore throats
- Most coughs
- Bronchitis
On the other hand, illnesses caused by bacteria, such as strep throat or a urinary tract infection, will respond to antibiotic therapy. In some cases, sinus infections and ear infections may also be treated with an antibiotic.
Antibiotics: Unnecessary use can be dangerous
You might think there’s no harm in taking an antibiotic if you have a viral infection, but that’s not true.
Taking antibiotics for any reason increases the risk that you will become resistant to antibiotic treatment later in life. In fact, as people have increasingly been treated with antibiotics over the last few decades, dangerous antibiotic resistance has been on the rise.
Antibiotic resistance is a worldwide problem, one that’s leading researchers to try and develop new, more potent medications to treat common bacterial infections. Antibiotic resistance costs $20 billion globally each year.
Do you remember hearing that a certain ingredient was being banned from hand soaps? That ingredient, triclosan, was found to contribute to antibiotic resistance, which is why it was banned by the FDA.
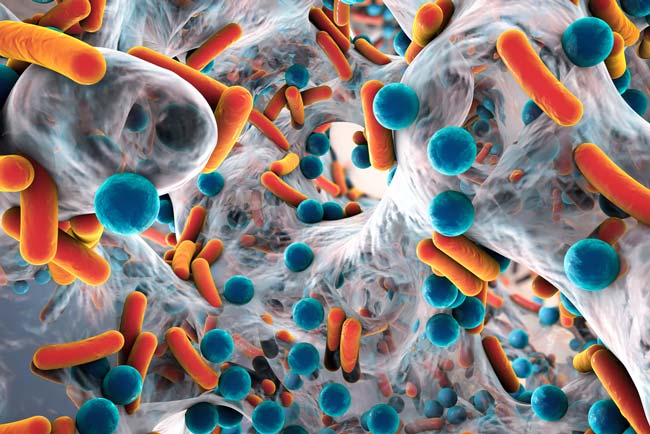
Beyond resistance, other problems can occur with antibiotic use. Antibiotics attack bacteria, and they kill off good bacteria in the body along with the bad.
Antibiotics also have a number of side effects, so using them when they’re unnecessary can lead to additional issues. In fact, antibiotics cause one in five ER visits related to adverse drug events.
Antibiotics: Different ones treat different bacteria
Antibiotics are not one-size-fits-all. Saving your “leftover” antibiotic for the next time you’re sick isn’t a good idea.
Proper treatment using an antibiotic requires knowing what type of bacteria is affecting the body. An antibiotic used to treat a urinary tract infection, for example, would be ineffective in treating strep throat.
In fact, for some illnesses, like a UTI, antibiotics are selected specifically based on the type of bacteria causing the infection. Treatment with an antibiotic formulated to treat a different type of bacteria would have no effect in treating another type of bacteria.
That’s why you shouldn’t take leftover antibiotics — and you shouldn’t take antibiotics prescribed for someone else. Taking the wrong kind can do more harm than good.
Not sure if an antibiotic will help your illness? Your doctor is the best person to make that call. Need a doctor? Find one here.